Abstract
Quality assurance (QA) plays a critical role in pharmaceutical compounding as it ensures the quality and safety of compounded preparations. Among the nine components outlined in USP chapter <1163>, verification is an essential part of the QA program. The verification process entails evaluating compounding facilities, equipment, methods, individual components, and final preparations, among other factors. It is crucial to ensure the quality of the active pharmaceutical ingredients (APIs) to maintain the integrity of compounded preparations. This involves first verifying the manufacturer's Certificate of Analysis (CoA). Incoming materials should be kept in a separate area (quarantine) pending CoA verification to prevent unintended use in the pharmacy. This editorial (QA Part 1) specifically focuses on the verification process and two pivotal parameters (Purity and expiration date) repoted in CoA.
Keywords: Compounding, Verification, Certificate of Analysis (CoA), Quality assurance, Purity, and expiration date.
Introduction
The quality, safety, and effectiveness of compounded preparations rely on the correct selection of ingredients. QA is a system that guarantees consistent adherence to quality standards within the compounding process.1,2 The USP monograph outlines the expectations for a medicine’s identity, strength, purity, and performance. It also includes the required tests to ensure that the medicine and its ingredients meet these expectations. A CoA is a report provided by a supplier/manufacturer that includes a description of the material, specifications, specific test results, expiration/retest date, etc. USP standards play a crucial role in preventing errors in compounding.3,4 According to USP <1163>, there are nine components of the QA program in pharmaceutical compounding such as “(1) Training (2) SOPs (3) Documentation (4) Verification (5) Testing (6) Cleaning, disinfecting, and safety (7) Containers, packaging, repackaging, labeling, and storage (8) Outsourcing, if used, and (9) Responsible personnel”.5 Verification is one of the important components. The responsible personnel should verify the ingredients, equipment, facility, compounding process, final preparations, etc. as per the standards. The quality of API and excipients should be verified upon receipt. Failure to authenticate the CoA may have several consequences such as low product quality and patient safety.
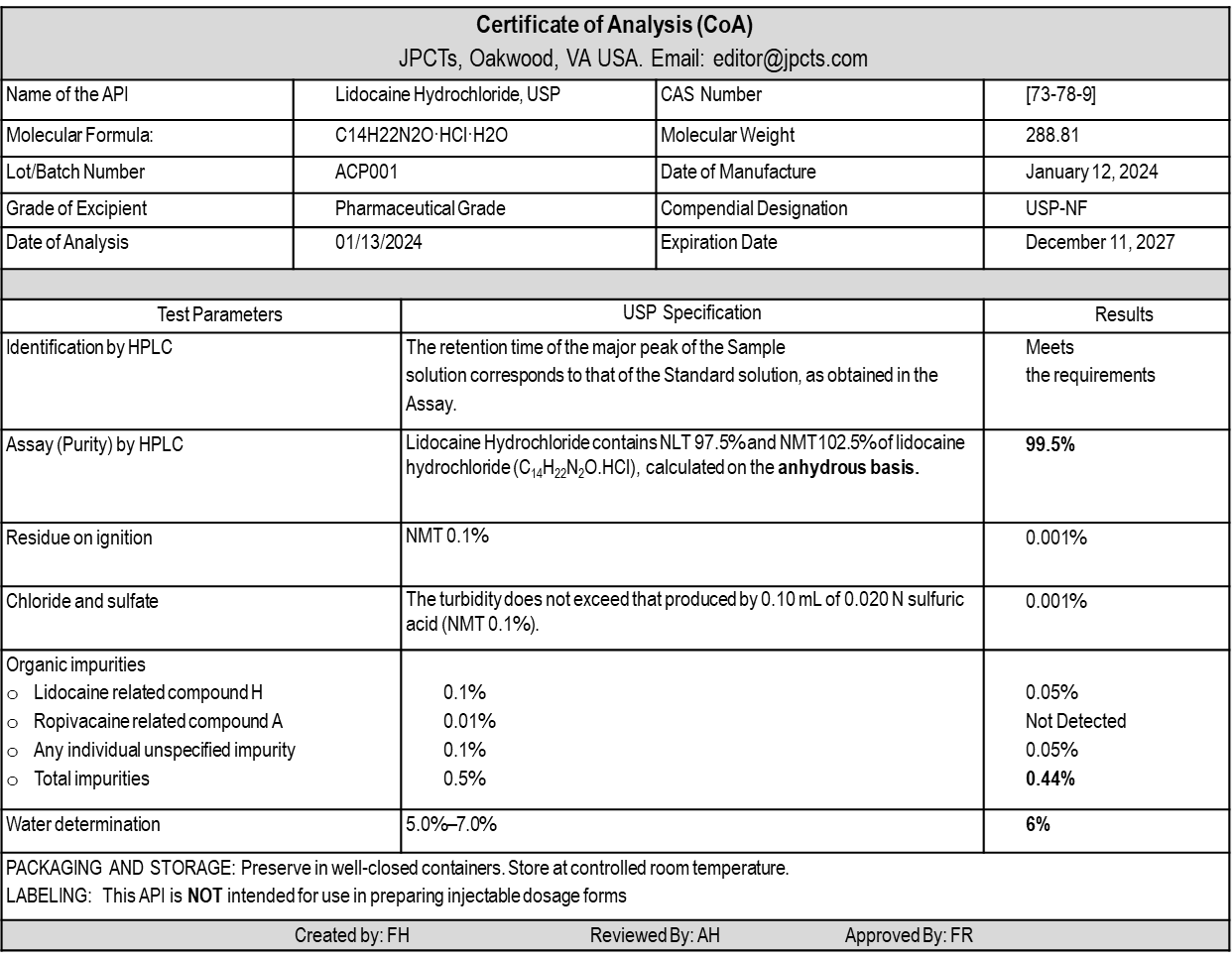
Table 1:
An Example of a CoA (Lidocaine Hydrochloride6)
Verification of manufacturer CoA is necessary:
- to ensure that the ingredient meets predetermined quality standards
- to mitigate error and risk
- to Compliance with Regulatory Requirements.
Unless otherwise specified, the Pharmacy should use pharmaceutical-grade ingredients manufactured in a cGMP facility to compound preparations. When API and excipients (inactive ingredients) are received, it is necessary to review the CoA to ensure that the ingredients meet the acceptance criteria stated in a relevant USP-NF monograph, if available. It is important for compounding personnel to have a clear understanding of the terminology used in CoA and USP monographs, including terms like identification, assay (purity), impurity profiles (organic impurities, inorganic impurities), residual solvents, water content, microbial limits, and more. In this section, the editor emphasizes the significance of two key parameters: %Assay (Purity) and expiration date. An example of CoA is represented in Table 1. This CoA confirms that the API (lidocaine hydrochloride) meets the standard requirements and is safe for use in compounded pharmaceuticals.
An assay is a test conducted to determine the presence and concentration of a specific substance. The most commonly used methods for this type of testing are High-Performance Liquid Chromatography (HPLC) and Potentiometry. It is important for compounding personnel to have a clear understanding of the term “%Assay (Purity)”. There are two ways in which %Assay can be reported in a Certificate of Analysis (CoA): “as-is basis” and “anhydrous basis” (See Table 2). For example, a %Assay of Lidocaine hydrochloride monohydrate for one specific batch on an as-is basis of 93.5% could mean that the API contains 93.5% Lidocaine hydrochloride, 6% water, and ~0.5% other materials such as impurities. The assay on an anhydrous basis is a calculated value derived from separate assay and water content tests. The industry-accepted formula for calculating the assay on an anhydrous basis is (assay on as-is basis × 100) / (100 – %water).7 This calculation takes into account the water content in the API. For example, if the as-is basis assay is 93.5% and the water content is 6%, the calculated assay on an anhydrous basis would be (93.5 × 100) / (100 – 6) = 99.47%. The %Assay (Purity) parameter is important because it helps compounders adjust the amount of API required for compounding when the potency falls below 100% but within the range as per the approved specification.
Table 2:
Comparison of the Base (Active Drug Moiety) and Salt forms of Lidocaine.

Additionally, it is important to verify whether the API is in base form (e.g., Lidocaine) or salt form (e.g., Lidocaine Hydrochloride) and if the salt form contains water of crystallization (a hydrate form). Hydrate forms of APIs are quite common, and the water molecules must be accounted for in the chemical formula. The base or active drug moeity of a drug is responsible for the pharmacological activity. To ensure stability, solubility, and other important physicochemical properties, the pharmaceutical manufacturer converts the base into a suitable soluble form. It is important for compounders/pharmacists to always consider the potential impact on the performance of a compounded drug product when there are differences in physical and chemical properties, such as solubility and stability, between the anhydrous and hydrate forms of the active drug substance.8
Expressing a drug’s strength or concentration of its active ingredient(s)/active moiety can be done in various ways such as percentages, milligrams per gram, milligrams per milliliter, etc. If the pharmacy has the salt form in stock and the prescription strength is based on the base form, the compounder needs to adjust the API weight by calculating the conversion factor (base to Salt or salt to base) using the molecular weights to obtain the correct strength. The editor suggests that the compounder should adjust the weight of the active drug required for compounding using the %Assay (on anhydrous basis) purity factor first. This adjustment should be made every time based on the purity of the API. If the compounder uses a salt form instead of the base form of the API, they should use the conversion factor as discussed above (Table 2) to calculate the amount of salt required to achieve the correct strength/dose.
The following calculation steps can be followed to calculate the theoretical weight of an ingredient in a compounded preparation:
Step 1: Calculate the Content of BASE required for the product.
For example, to compound 50 grams of the 2% lidocaine topical gel, 1000 mg of lidocaine is needed.
Step 2: Adjust the weight (calculated in Step 1) using the %Assay value.
For example, if the purity of anhydrous lidocaine is 99.5%, the compounder should adjust the weight (1000 mg) by dividing it by the purity factor (0.995). This results in a calculated amount of 1005.025 mg, which should be used instead of the initial 1000 mg to ensure high-quality preparations.
Note: No action is required when the %Assay is more than 100%.”
Step 3: Base to Salt conversion
For example, if the pharmacy has the salt form (Lidocaine Hydrochloride monohydrate) in stock, the compounder should adjust the API weight by dividing the weight (Step 2) by the conversion factor (0.81 *See Table 2). This results in a calculated amount of 1240.772 mg of Lidocaine Hydrochloride monohydrate, which should be used to ensure the high quality and correct strength of the preparation.
Beyond Use Date (BUD) and expiration dates are distinct concepts. The expiration date signifies the period within which a manufactured product, API, or added substance is anticipated to meet specified requirements outlined in a compendial monograph, if available, and if it is stored under recommended conditions. On the other hand, the BUD is the date or time after which a compounded preparation should not be used and is calculated from the day and time of compounding. The author suggests that if an API does not come with an expiration date from the supplier, pharmacy personnel should either contact the supplier to request a Certificate of Analysis (CoA) with a retest or expiration date or return the API to the supplier or reject it. According to the current USP <795> standard, inactive ingredients can be used in compounding non-sterile preparations without a vendor expiration date for up to 3 years from the date of receipt unless the ingredient is known to be susceptible to degradation. In the case of degradation-prone ingredients, a shorter expiration date should be assigned according to USP <797> Chapter. 3
As the USP chapters are a minimum standard, the editor believes that compounding pharmacies and state regulators should reevaluate the standard regarding the expiration date of inactive ingredients and can enforce more stringent requirements for the following reasons:
- The absence of an expiration date on CoA suggests that the ingredients were most likely not manufactured in a cGMP facility or that the manufacturer did not follow common standard practices.
- There is a chance that the pharmacy may receive the ingredient at the end of its shelf life.
- Some inactive ingredients, such as lactose, colors, and flavors, are prone to degradation and have a shorter shelf life (usually 1-2 years).9
- Additionally, in real-life scenarios, considering the workload in the pharmacy,10 the compounder can make a mistake in determining whether an ingredient is susceptible to degradation or not.
Conclusion
Before compounding any preparation, responsible personnel should verify the expiration dates of all ingredients, as well as the purity (%Assay) of the API, and record this information in the Compounding Records. The verification of manufacturer CoA with the USP Monograph specifications is one of the initial processes in ensuring the safety, efficacy, and compliance of compounded preparations. Any component of unacceptable quality must be promptly rejected and separated from active stock to prevent unintended use and finally discarded properly. Compounding pharmacies, and regulatory bodies should enforce this key practice to minimize compounding error and confirm the highest standards of compounding practice to ensure patient safety.
Acknowledgments
The editor is thankful to Mr. A.H.M. Arif Ur Rashid, Sr. Assistant Manager, QC, Beximco Pharmaceuticals Ltd, Bangladesh for his time and effort in reviewing this editorial.
Conflict of interest
The authors declare no Conflict of interest.
References
- Hall E, Levesque D, Rashid M, Mullins R, Hossain MF. A Simplified Method for Compounding Lidocaine Topical Gel: A Demonstration of Quality Assurance to Prevent Errors in 503A Pharmacies. Int J Pharm Compd. 2021;25(3):197-204. [PubMed]
- Hossain MF. Compounding Lidocaine Topical Gel: An Exhibit of a “Master Formulation and Compounding Records” for 503A pharmacies. J Pharm Compd Ther. 2024;1(1):1-5. [Link]
- United States Pharmacopeial Convention, Inc. General Chapter <795> Pharmaceutical Compounding – Nonsterile Preparations. Accessed January 2, 2024. [Link]
- United States Pharmacopeial Convention, Inc. General Chapter <797> Pharmaceutical Compounding – Sterile Preparations. Accessed January 2, 2024. [Link]
- United States Pharmacopeial Convention, Inc. General Chapter 〈1163〉 Quality Assurance in Pharmaceutical Compounding. Accessed January 2, 2024. [Link]
- United States Pharmacopeial Convention, Inc. Official Monographs/Lidocaine Hydrochloride. Accessed January 3, 2024. [Link]
- Shivram K, Patil DM, Shah ND, Thite RU, Joshi AS, Motka NP. An Unrealistic Drift in Assay on Anhydrous Basis towards Content Limit. Indian J Pharm Sci. 2009;71(6):679-684. doi:10.4103/0250-474X.59553 [PubMed]
- US FDA. Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act. Published online September 29, 2023. Accessed January 19, 2024. [Link]
- Spectrum Chemical Lactose, Monohydrate, Powder, Reagent ACS Grade; 12 kg from Cole-Parmer. Accessed January 19, 2024. [Link]
- Chui MA, Mott DA. Community Pharmacists’ Subjective Workload and Perceived Task Performance: a Human Factors Approach. J Am Pharm Assoc JAPhA. 2012;52(6):e153-e160. [PubMed]
Quality Assurance in Pharmaceutical Compounding (QA Part 1): Verification of Certificate of Analysis (CoA) by Mohammad Faisal Hossain is licensed under CC BY 4.0
Note
Copyright © 2024 Hossain. Place of Publication: PSciP Publishing LLC, Oakwood, VA, USA.
